It is deeply worrying for parents to watch their child struggle with focus, restlessness, or unpredictable mood swings. ADHD is often the first explanation parents hear. However, attention and behavior changes are not always neurodevelopmental. In many cases, low iron levels can mimic, contribute to, or worsen symptoms that resemble ADHD. Therefore, differentiating between ADHD vs. iron deficiency in children is essential.
Iron is the brain’s “fuel for focus.” It plays a vital role in dopamine production and energy regulation. When ferritin levels (the body’s iron stores) are low, the brain essentially runs on a “low battery,” leading to poor concentration and irritability. Understanding these differences ensures that a child is not treated for a disorder when they actually have a treatable nutritional gap.
If your child shows persistent restlessness, mood swings, or difficulty concentrating, look beyond brain chemistry and consider potential nutritional gaps. In this article, we explore the scientific link between ADHD and iron deficiency in children, highlighting seven key signs that may help distinguish whether a child’s symptoms stem from iron levels or a primary neurodevelopmental condition.
⚡ Executive Summary:
- The Biological Link: Iron is essential for dopamine activity. Low levels can mimic ADHD-like traits by affecting brain energy metabolism.
- Overlapping Symptoms: Both conditions can present with inattention and restlessness, making it difficult to distinguish them based on behavior analysis alone.
- The Physical Clues: Unlike ADHD, iron deficiency often includes persistent fatigue, pale skin, or pica (cravings for ice).
- The Diagnostic Gap: A full iron panel (along with serum ferritin) is vital. Hemoglobin may appear normal even when ferritin (stored iron) is low.
- The Bottom Line: Ruling out a medical gap first ensures your child receives the most effective support.
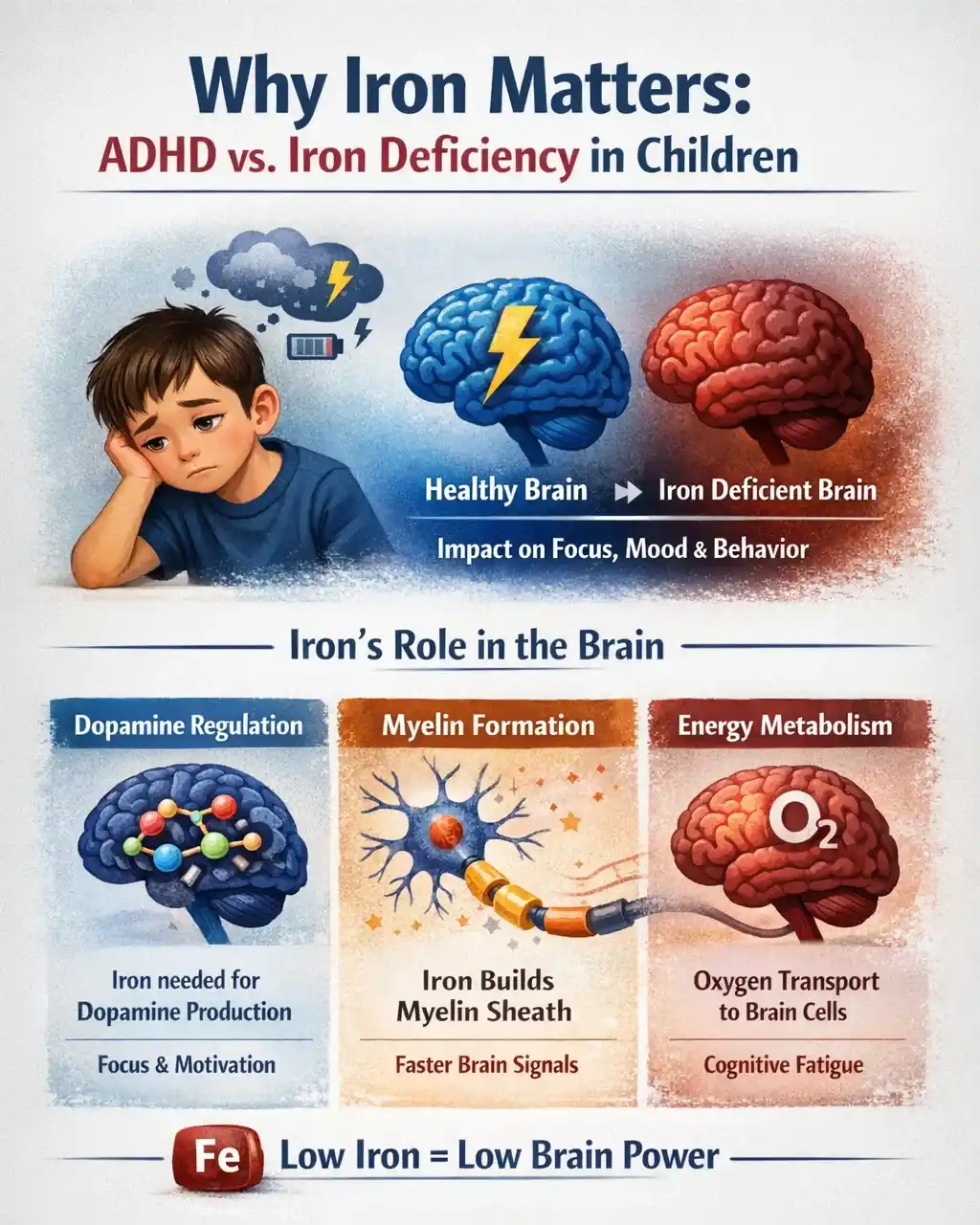
Why Iron Matters for the Brain
Iron is essential for healthy brain function. Since the brain requires high energy, low iron can affect how a child thinks and behaves.
Iron Supports
- Dopamine Regulation: Iron is a necessary co‑factor for synthesis of dopamine. Dopamine is the brain chemical most closely linked to focus, motivation, and behavioral control.1
- Myelin Formation: It supports the development of myelin, the protective coating around nerves that allows brain signals to travel at high speeds.2
- Energy Metabolism: Iron carries oxygen to the brain’s cells. In its absence, the brain essentially “runs on a low battery,” triggering significant cognitive fatigue.3
When iron is low, the nervous system may struggle to stay balanced. As a result, behaviors can look similar to ADHD.
The “Mirror Effect”: How Iron Deficiency Mimics ADHD Symptoms in Kids
Because iron is a critical co-factor for the enzyme that produces dopamine, a deficiency can disrupt key dopaminergic pathways.4 This is significant because ADHD is also characterized by dysregulated dopamine pathways, particularly in the brain’s reward and attention centers.
When the nervous system lacks this essential mineral support, it struggles to maintain neurochemical balance. This may create a “mirror effect,” where a child’s behaviors look very similar to ADHD. In a clinical setting, these signs often include:
- Inattention: Difficulty focusing because the brain is deprived of oxygen and dopamine.
- Regulation Issues: Restlessness or irritability as the nervous system falters without adequate myelin support.
- Emotional Volatility: Sudden mood swings triggered by energy “crashes” throughout the day.
- Physical Exhaustion: Appearing “lazy” or unmotivated, when in reality they are experiencing profound fatigue.
Parent Note: These symptoms alone are not a diagnosis. However, if your child shows ADHD-like behaviors alongside physical signs like pale skin, cold hands/feet, or frequent exhaustion, a full iron panel (including a ferritin test) is a wise first step.
🔗 Related: If your child’s focus issues are paired with growth changes or temperature sensitivity, you should also ask: Is It ADHD or a Thyroid Condition? Explore the 7 Hidden Signs of Misdiagnosis to check whether a hormonal imbalance may be contributing.
Research Evidence: Pediatric ADHD and Low Iron Link
Over the past decade, clinical data has confirmed the link between iron deficiency and ADHD symptoms in children, highlighting how metabolic health impacts neurological behavior.
Key Research Findings: ADHD vs. Iron Deficiency in Children
- Lower ferritin levels in ADHD: Multiple studies, including a 2018 study published in Nature and a 2020 meta-analysis of 17 studies, have confirmed that children with ADHD often show lower serum ferritin levels, suggesting that iron deficiency may affect attention and behavior.5, 6
- Increased ADHD diagnosis risk: Research published in the Indian Journal of Psychiatry found that children with iron deficiency anemia were 3.82 times more likely to be diagnosed with ADHD.7
- Long-term developmental impact: A 2024 longitudinal study showed that iron deficiency in infancy can have lasting effects on brain development, increasing the risk of sluggish cognitive tempo and ADHD symptoms later in childhood and adolescence.8
- Broader nutrient links: In addition, researchers found that not only low serum iron and ferritin, but also vitamin D, thyroid, and magnesium deficiency were clearly associated with higher rates of hyperactivity, inattention, and impulsivity.9, 10, 11
The Bottom Line: These findings show a strong association, not direct cause. While iron deficiency does not “create” ADHD, it can certainly mimic or significantly worsen the symptoms.
Red Flags: 7 Hidden Signs That Distinguish Iron Deficiency from ADHD
If your child exhibits focus or behavioral issues, these “Red Flags” can help you determine if the root cause is nutritional rather than neurodevelopmental.
Quick Overview: ADHD vs. Iron Deficiency Symptoms
Feature Iron Deficiency Pattern ADHD Pattern The Key Difference Energy Levels Child feels tired, sluggish, or drained, even after rest. Normal to high energy; child often feels "driven by a motor." Persistent physical tiredness points to iron deficiency. Concentration Brain fog" caused by low oxygen and reduced dopamine. Distractibility; mind jumps from one interest to another. If focus improves with nutrition, it likely wasn't ADHD. Mood Irritability triggered by metabolic energy crashes. Emotional outbursts linked to low frustration tolerance. Mood swings tied to fatigue suggest iron deficiency. Restlessness Jitteriness or "creepy-crawly" leg feelings (RLS). Persistent, behavioral hyperactivity and fidgeting. Restlessness with physical signs points to iron. Cognition Slowed thinking and "lagging" cognitive processing. Rapid, divergent thinking that is easily interrupted. Complaints of mental slowness are unique to iron deficiency. Sleep Disrupted cycles; thrashing or trouble staying asleep. Racing mind; primarily trouble falling asleep. Sleep issues pre-treatment point strongly to low iron. Physical Signs Pale skin, brittle nails, or cravings for ice/dirt. No specific physical changes in appearance. Visible physical clues are the "smoking gun" for iron.
Red Flag #1: Low Energy and Constant Fatigue
Children with iron deficiency often feel drained or unmotivated because their brains are not getting enough oxygen. They may avoid active play or struggle to keep up with peers.
- ADHD Pattern: ADHD itself is not a medical cause of low energy levels. While children may feel mentally exhausted from effortful focus, they typically maintain high or normal physical energy.
- The Clue: Persistent physical tiredness points toward a nutritional deficiency, not a neurodevelopmental one.
Red Flag #2: Trouble Concentrating and “Brain Fog”
Low iron disrupts the supply of dopamine and oxygen, causing children to stare blankly or describe their thinking as “slow” or “cloudy.”
- ADHD Pattern: While inattention is a hallmark of ADHD, it stems from regulation differences—children rarely describe their actual thoughts as feeling “foggy.”
- The Clue: If mental clarity fluctuates or improves significantly after rest or high-iron meals, it likely is not primary ADHD.
Red Flag #3: Irritability and the “Daily Crash”
An iron deficiency causes energy drops throughout the day, which can trigger irritability, frustration, or emotional outbursts
- ADHD Pattern: Emotional dysregulation in ADHD is usually linked to impulsivity and difficulty managing frustration, rather than metabolic shifts in energy.
- The Clue: Mood swings tied specifically to physical fatigue or the “afternoon slump” suggest iron deficiency.
Red Flag #4: Restlessness and Fidgeting
When iron is low, the nervous system struggles to regulate itself, causing jitteriness, foot-tapping, or constant “creepy-crawly” feelings in the limbs.
- ADHD Pattern: Hyperactivity in ADHD is persistent and behavioral; it doesn’t typically increase or decrease based on nutritional status or physical fatigue.
- The Clue: Restlessness paired with other physical markers (like paleness) strongly suggests a deficiency.
🔗 Related: If your child is constantly fidgeting or unable to relax their body at night, you may want to explore the role of minerals in behavior. Read our latest guide: Magnesium for ADHD in Children: Can This Mineral Calm Hyperactivity? to learn how magnesium may support calmer sleep and improved focus.
Red Flag #5: Forgetfulness and Slowed Thinking
Low iron slows cognitive processing, making children forgetful, mentally “foggy,” or slow to respond. Homework may be lost, instructions forgotten, and tasks take longer.
- ADHD Pattern: A child with ADHD may be distracted by something else, but their actual processing speed is often quite fast.
- The Clue: A “slow to respond” or “mentally sluggish” memory is more consistent with a biological fuel shortage.
Red Flag #6: Sleep Difficulties
Iron deficiency is a leading cause of Restless Leg Syndrome (RLS) and sleep fragmentation. Poor sleep then creates a vicious cycle of daytime focus problems.
- ADHD Pattern: Sleep problems are common in ADHD, but they usually involve a “busy brain” that won’t shut off, rather than physical discomfort in the legs.
- The Clue: Sleep issues present before any ADHD treatment are a major red flag for low iron.
Red Flag #7: Physical Signs Beyond Behavior
Iron deficiency shows physical signs that ADHD simply cannot explain. Watch for pale skin (especially inside the lower eyelids), brittle nails, or pica (unusual cravings for non-food items like chewing ice, dirt, or paper).
- ADHD Pattern: ADHD is a neurodevelopmental condition and does not directly cause physical symptoms like pallor or brittle nails.
- The Clue: Physical markers provide the most objective evidence that you should request a full iron blood panel.
How to Rule Out Iron Deficiency Before an ADHD Diagnosis: Action Checklist
Before proceeding with an ADHD evaluation, follow this structured path to ensure your child’s symptoms are not actually a treatable biological gap.
Step 1: The Home Evidence Log
Gather at least 3–5 days of data to share with your doctor.
- Energy Tracking: Note the time of day when focus is at its worst. Is it consistent throughout the day (ADHD), or does it plummet in the afternoon (Iron)?
- The Physical Check: Inspect your child’s nails (are they brittle or spoon-shaped?), inner eyelids (are they pale?), and skin tone.
- The Timing Log: Note if behaviors worsen in the late afternoon or after school (the “daily crash”).
- The Diet Review: Calculate daily cow’s milk intake and check for “pica” (e.g., chewing on ice or paper).
- Sleep Observation: Does your child kick their legs, toss and turn, or complain of “growing pains” at night?
Step 2: The Pediatric Appointment (The Lab Request)
Do not just ask for “blood work.” Be specific to avoid incomplete results.
- Request a “Full Iron Panel”: Specifically ask for Serum Ferritin and Iron Saturation. Remind the doctor that you want to check iron stores (Ferritin), not just the iron currently circulating in the blood (Hemoglobin).
- C-Reactive Protein (CRP): A marker of inflammation. If CRP is high, it can cause a “false normal” ferritin reading even if your child is deficient.
- Thyroid Screen: To rule out thyroid-related focus and energy issues.
Step 3: Post-Test Strategy
If a deficiency is found, follow this path before revisiting an ADHD diagnosis.
- Supplementation: Follow the exact dosage prescribed by your doctor.
- Vitamin C Pairing: Administer iron with a source of Vitamin C (like orange juice) to significantly increase absorption.
- The 3-Month Re-Test: Schedule follow-up blood work for 90 days out. It takes this long for the body to build new red blood cells and replenish brain stores.
- The Symptom Re-Evaluation: After 3–6 months of optimized levels, review the “Red Flags.” If focus and mood have improved, the root cause was likely nutritional.
⚠️ Critical Safety Reminder:
Never start an iron supplement without a doctor’s supervision. Iron is a powerful mineral, and excess iron can be harmful. Your pediatrician will use blood panel results to calculate the exact dosage your child needs.
Takeaway
ADHD and iron deficiency can look very similar, but they are not the same. While ADHD is neurodevelopmental, iron deficiency is a treatable medical gap that can directly influence brain function.
Low iron often acts as an “amplifier,” making ADHD symptoms feel more intense and harder to manage. By identifying and correcting a deficiency via a Full Iron Panel (Ferritin + Saturation), you clarify the full picture of your child’s needs.
Always rule out nutritional gaps before finalizing a neurodevelopmental diagnosis. Addressing the biological foundation ensures that treatable contributors aren’t missed, giving your child the best chance to feel focused, energetic, and balanced.
🧠 ADHD vs. Iron Deficiency Tracker
Parent’s Tool to Identifying Nutritional Mimics
1Energy & Metabolic Log
2Physical “Red Flags”
If two or more signs are present, ask your pediatrician about a Full Iron Panel (including Ferritin).
📊 Lab Results Tracker
| Test Marker | Result | Optimal Range (May vary) |
|---|---|---|
| Hemoglobin | ______ | 11.5–15 g/dL |
| Serum Ferritin | ______ | 50 – 100 ng/mL |
| Iron Saturation | ______ | 20–50% |
Consult your physician before beginning supplements.
Frequently Asked Questions
Q1. Can a child have both ADHD and iron deficiency?
Yes, a child can have both. Iron deficiency may worsen attention and behavioral issues in children who also have ADHD, so identifying and correcting deficiencies is important for overall management.
Q2. Can iron deficiency really mimic ADHD symptoms in children?
Yes. Iron is essential for dopamine production and brain oxygenation. When iron is low, children often exhibit inattentiveness, irritability, and restlessness, leading to frequent ADHD misdiagnosis or confusion with child focus issues.7
Q3. What are the key differences between ADHD and iron deficiency behaviors?
The main difference is energy levels. ADHD typically features normal-to-high energy (“driven by a motor”), whereas iron deficiency causes physical fatigue and brain fog. If a child is inattentive and physically drained, it points toward a nutritional cause.
Q4. Which blood tests should parents request for a proper evaluation?
A standard CBC is often not enough. Parents should request a pediatric iron panel that specifically includes Serum Ferritin (to check iron stores) and Iron Saturation. This ensures a comprehensive ADHD evaluation that rules out biological mimics.
Q5. Can a child have normal hemoglobin but still be iron deficient?
Absolutely. This is known as “non-anemic iron deficiency.” A child may have normal hemoglobin but low ferritin, meaning their blood count looks fine, but their brain lacks the stored iron necessary for optimal child brain health.
Q6. What physical signs suggest iron deficiency beyond behavior changes?
Look for ADHD look-alike symptoms paired with physical markers like pallor (paleness), brittle nails, or pica (craving ice or non-food items). ADHD is purely neurodevelopmental and does not cause these physical changes.
Q7. How does low iron affect dopamine and brain function?
Iron is a co-factor for the enzyme that creates dopamine. Without it, iron dopamine regulation is disrupted, slowing down brain function and leading to the distractibility and impulsivity commonly associated with ADHD brain chemistry.
Q8. When should iron testing not be delayed?
Urgent iron testing is recommended if focus issues are accompanied by restless sleep, chronic fatigue, or if the child has a high intake of “iron-blockers” like excessive cow’s milk. Always request an iron panel before finalizing an ADHD diagnosis.
References
📚 Click to view references
- Robberecht H, Verlaet AAJ, Breynaert A, De Bruyne T, Hermans N.: Magnesium, Iron, Zinc, Copper and Selenium Status in Attention-Deficit/Hyperactivity Disorder (ADHD). Molecules. 2020;25(19):4440.Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC7583976/
- Connor JR, Menzies SL.: Relationship of iron to oligodendrocytes and myelination. Glia. 1996;17(2):83–93. Available from: https://pubmed.ncbi.nlm.nih.gov/8776576/
- Kim SL, Shin S, Yang SJ: Iron Homeostasis and Energy Metabolism in Obesity.
Clinical Nutrition Research. 2022;11(4):316–330. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC9633967/
- Gkotsoulias DG, Rullmann M, Schmitt S, Bujanow A, Zientek F, Messerschmidt K, Pampel A, Büttner AP, Schildan A, Sabri O, Müller-Vahl K, Barthel H, Möller HE. Abnormalities of iron homeostasis and the dopaminergic system in Tourette syndrome revealed by 7T MRI and PET. Brain Commun. 2025 Mar 10;7(2):fcaf104. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC11961303/
- Tseng PT et al. (2018).: Peripheral iron levels in children with attention-deficit hyperactivity disorder: A systematic review and meta-analysis. Scientific Reports. Available from: https://www.nature.com/articles/s41598-017-19096-x
- Anand B, Sireesha CV. (2022).: Lower serum ferritin levels and higher inattentiveness in attention deficit hyperactivity disorder. Archives of Mental Health, 23(2), 95–100. Available from: https://doi.org/10.4103/amh.amh_19_22
- Islam K, Seth S, Saha S, Roy A, Das R, Datta AK. (2018).: A study on association of iron deficiency with attention deficit hyperactivity disorder in a tertiary care center. Indian Journal of Psychiatry, 60(1), 131–134. Available from: https://doi.org/10.4103/psychiatry.IndianJPsychiatry_197_17
- East PL, Doom JR, Blanco E, Burrows R, Lozoff B, Gahagan S.: Iron Deficiency in Infancy and Sluggish Cognitive Tempo and ADHD Symptoms in Childhood and Adolescence. J Clin Child Adolesc Psychol. 2023;52(2):259–270. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC8918441/
- Bener A, Kamal M, Bener H, Bhugra D.: Higher prevalence of iron deficiency as strong predictor of attention deficit hyperactivity disorder in children. Ann Med Health Sci Res. 2014;4 (Suppl 3):S291–S297. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC4212392/
- Chen G, Gao W, Xu Y, Chen H, Cai H. Serum TSH Levels are Associated with Hyperactivity Behaviors in Children with Attention Deficit/Hyperactivity Disorder. Neuropsychiatr Dis Treat. 2023 Mar 7;19:557-564. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC10007977/
- Hunter C, Smith C, Davies E, Dyall SC, Gow RV. A closer look at the role of nutrition in children and adults with ADHD and neurodivergence. Front Nutr. 2025 Jul 30;12:1586925. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC12343232/