Many parents ask the same hopeful question: “Can ADHD be detected by a blood test?”
The short answer is no. ADHD is a clinical diagnosis based on a child’s developmental history and behavioral patterns, and there is currently no single biological marker that can confirm or rule it out.
However, updated 2026 clinical guidelines note that certain blood tests for ADHD in children can provide valuable insights before starting medication. These tests help identify “ADHD mimics”—medical conditions or nutrient deficiencies that resemble ADHD symptoms but require different care.
In this post, we highlight 7 essential ADHD blood tests that parents and clinicians often consider to support a more accurate diagnosis and a safer, more effective treatment approach.
💡 EXECUTIVE SUMMARY
While ADHD is a clinical diagnosis, it has a deep biological foundation. Testing for key blood markers is not about “detecting” ADHD; it is about ruling out medical mimics and ensuring the brain has the biochemical precursors required for focus and medication efficacy.
📋 Markers commonly reviewed include:
- Thyroid Panel: Rules out metabolic “mimics” causing restlessness.
- Ferritin (Iron): Vital fuel for dopamine synthesis.
- Zinc: A key co-factor for focus and stimulant medication response.
- Vitamin D: Supports mood regulation and cognitive processing speed.
- B-Vitamins: Drives the methylation cycle for neurotransmitter repair.
- RBC Magnesium: The “calmative” mineral for the nervous system and sleep.
- Diabetes Profile: Prevents impulsivity caused by blood sugar crashes.
Why Blood Tests are Recommended Before Starting ADHD Medication
ADHD (Attention-Deficit/Hyperactivity Disorder) is a neurodevelopmental condition. However, its core symptoms can overlap with treatable medical issues such as thyroid dysfunction, iron deficiency, or blood sugar imbalance.
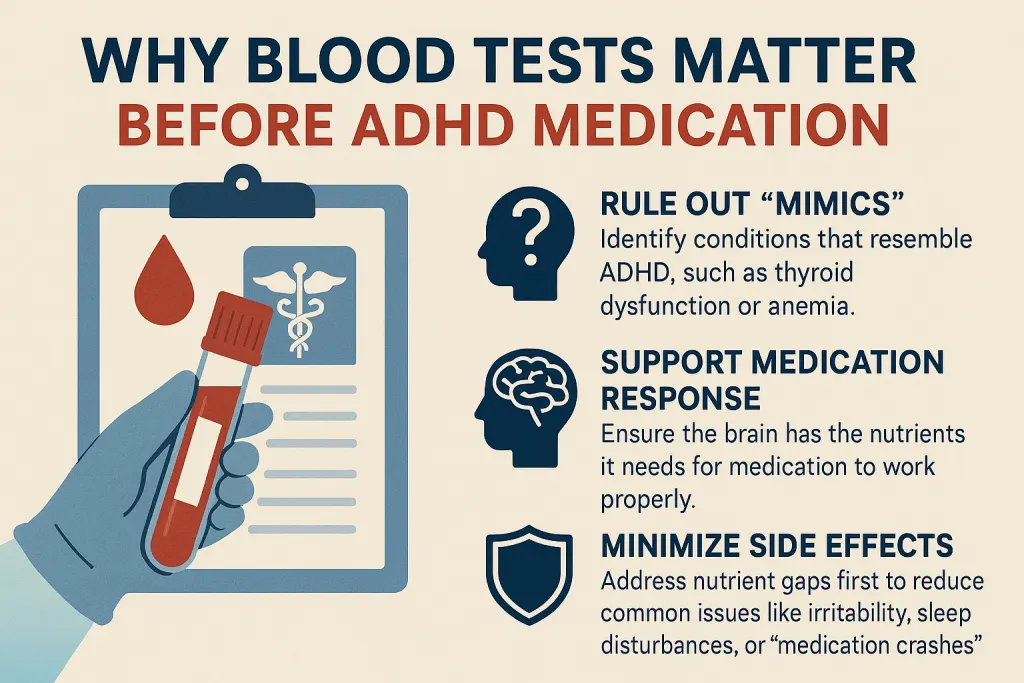
Some clinicians recommend baseline blood work before starting stimulant or non-stimulant medication. These tests do not diagnose ADHD, but they can support care in three ways.
1. Rule Out “Symptom Mimics”
The primary purpose of an ADHD blood test is to detect medical conditions that mimic ADHD—such as thyroid disorders or anemia. If a child is labeled with ADHD but the underlying issue is a thyroid imbalance, medication may be ineffective because the true root cause remains untreated.
2. Support Medication Response
The brain is a chemical factory. It requires specific “raw materials” like zinc, iron, and magnesium to produce neurotransmitters like dopamine. If these levels are low, ADHD medications—which rely on those same neurotransmitters—may be less effective. Testing ensures the brain has the “biological fuel” it needs.
3. Minimize Med Side Effects
Starting medication on a “depleted” system often leads to a rougher experience. For example, a child with unstable blood sugar might experience a much more severe “medication crash” such as:
- Increased irritability or “moodiness.”
- Sleep disturbances and difficulty falling asleep.
- Severe “rebound” symptoms as medication wears off.
Correcting nutrient and glucose gaps first can help reduce these effects.
What to Test: The 7 Essential Blood Tests For ADHD In Children
Here is the 7 Essential ADHD Blood Test Checklist every parent should know.
Marker Why It Matters Optimal Target for ADHD and Focus 1. Thyroid (Full Panel) Controls energy and mood; prevents ADHD "mimics." TSH: 1.0–2.5; FT3: 5.5–8 and FT4: 14–20 2. Ferritin Stores iron needed for Dopamine production. 50–100 ng/mL 3. Zinc (Plasma) Regulates dopamine and melatonin; supports sleep. 90 – 115 µg/dL 4. Vitamin D Acts as a neuro-steroid for focus and impulse control. 50 – 80 ng/mL 5. B12, Folate, & Homocysteine The "fuel" for neurotransmitter synthesis (Methylation). B12: 600–900 pg/mL; Folate (B9): 10 – 15 ng/mL; Homocysteine: < 8 6. RBC Magnesium The "brake" for the nervous system; reduces hyperactivity. 6.0 – 6.5 mg/dL 7. Diabetes Profile Prevents adrenaline spikes and focus "crashes." Glucose: 80–90 mg/dL; HbA1c: 4.8%–5.2%; Insulin: 2.0–6.0 uIU/mL
Note: Pediatric reference ranges may vary slightly by age. Always interpret results with your child’s doctor.
1. Thyroid Panel (TSH, Free T3/T4, TPO Antibodies)
Thyroid imbalance is one of the most common medical conditions misdiagnosed as ADHD in children. Because the thyroid gland regulates metabolism and brain energy, even small shifts in hormone levels can trigger symptoms that closely resemble ADHD.
- Hypothyroidism (Underactive): This condition causes “brain fog,” slow processing speed, and poor memory. These symptoms can be misinterpreted as the inattentive type of ADHD.
- Hyperthyroidism (Overactive): This condition creates restlessness, anxiety, and an inability to sit still. These symptoms can be confused with the hyperactive-Impulsive type of ADHD.
What to Ask Your Pediatrician
To get a complete picture, move beyond a simple TSH screening. Specifically, ask for these comprehensive markers:
- TSH: To see if the brain is signaling the thyroid correctly.
- Free T3 & Free T4: To measure the actual hormones available for brain function.
- TPO Antibodies: To rule out autoimmune-related cognitive symptoms.
Pediatric Thyroid Reference Range
Age Group TSH (mIU/L) Free T3 (pmol/L) Free T4 (pmol/L) Optimal Target for Focus 1–6 years 0.5 – 4.5 3.7 – 8.5 12.0 – 22.0 TSH closer to 1–2; Free T3 closer to 6.5–8.0; Free T4 closer to 17–20 7–12 years 0.5 – 4.5 3.9 – 8.0 11.5 – 20.0 TSH closer to 1–2; Free T3 closer to 6–7.5; Free T4 closer to 16–19 13–18 years 0.5 – 4.5 3.9 – 7.7 11.0 – 18.0 TSH closer to 1.5–2.5; Free T3 closer to 5.5–7.0; Free T4 closer to 14–17
🔗 Related Reading:
If your child’s focus issues are paired with growth changes or unusual temperature sensitivity, it may not be ADHD alone. You may want to ask: Is It ADHD or a Thyroid Condition?
2. CBC + Ferritin (Iron Stores)
Iron is essential for dopamine synthesis, the neurotransmitter responsible for focus, motivation, and executive function. When iron levels are low, the brain simply cannot produce enough dopamine to maintain attention.
- Sleep & Restlessness: Low ferritin is a primary contributor to restless legs and poor sleep quality. This leads to chronic exhaustion, which intensifies next-day inattention and irritability.
- Daily Energy: A deficiency often shows up as fatigue and a lack of motivation, which can look identical to “sluggish” ADHD-type inattention.
What to Ask Your Pediatrician
It is vital to request a Serum Ferritin test alongside a standard CBC (Complete Blood Count).
While the CBC checks for active anemia, the Ferritin test shows the body’s “iron savings account.” A child’s CBC can look “normal” even if their iron stores are nearly empty—a state that still significantly impacts brain function.
Pediatric Ferritin Reference Range
Age Group Lab “Normal” Range (ng/mL) Optimal Target for ADHD and Focus 1–6 years 15 – 200 Ferritin: 50 – 80 ng/mL 7–12 years 15 – 200 Ferritin: 50 – 90 ng/mL 13–18 years 20 – 250 Ferritin: 60 – 100 ng/mL
🔗 Related Reading:
If your child struggles with restless sleep or frequent leg movements at night, iron levels may be part of the picture. As a result, some children are misidentified. Read our guide: Is It ADHD or Iron Deficiency in Children? 7 Hidden Signs of Misdiagnosis.
3. Plasma Zinc
Zinc is an essential co-factor for dopamine regulation. Without adequate zinc, the brain struggles to use dopamine effectively, leading to significant challenges with attention, impulse control, and mood.
Zinc is also required for the body to absorb Vitamin B6. A deficiency in zinc can create a “hidden” B6 deficiency, resulting in irritability and a lower threshold for stress.
Furthermore, low zinc is linked to a poorer response to stimulant medications. Correcting this nutritional gap can often help medication work more effectively, sometimes allowing for optimal results at lower doses.
What to Ask Your Pediatrician
Request a Plasma Zinc test. For the most accurate results, this should be done as a fasting blood draw in the morning, as zinc levels fluctuate significantly after eating.
Pediatric Zinc Reference Range
Age Group Lab “Normal” Range (µg/dL) Optimal Target for ADHD and Focus 1–6 years 60 – 120 Zinc: 90 – 110 µg/dL 7–12 years 60 – 120 Zinc: 90 – 110 µg/dL 13–18 years 60 – 120 Zinc: 95 – 115 µg/dL
4. Vitamin D (25‑Hydroxy Test)
Vitamin D functions as a neuro‑steroid hormone, supporting nerve growth and regulating serotonin and dopamine.
Deficiency often leads to emotional dysregulation, irritability, low mood, and slower cognitive processing, symptoms that frequently overlap with ADHD.
What to Ask Your Pediatrician
Request a 25‑Hydroxy Vitamin D test (25‑OH D). This is the most accurate measure of your child’s actual Vitamin D stores.
Pediatric Vitamin D Reference Range
Category Lab “Normal” Range (ng/mL) Optimal Target for ADHD and Focus Bone Health Above 30 Prevents physical disease but may not support focus. Mental Health and Focus 30 – 100 Optimal: 50 – 80 ng/mL
5. Vitamin B12, Folate & Homocysteine (Methylation Panel)
B12 and Folate are essential for methylation, the biochemical process that builds and repairs neurotransmitters.
When methylation is slow, often due to the MTHFR gene mutation, the brain struggles to convert amino acids into dopamine, norepinephrine, and serotonin.
- Neurotransmitter Conversion: Without adequate B12 and Folate, the brain cannot efficiently convert amino acids into the dopamine and norepinephrine needed for focus.
- Stress & Anxiety: Sluggish methylation often results in high anxiety and low stress tolerance, overlapping with ADHD‑like emotional dysregulation.
What to Ask Your Pediatrician
A “normal” B12 result can be misleading. To see if the body is actually using these vitamins, request:
- Serum B12 & Folate: To check the current levels in the bloodstream.
- Homocysteine: This is the “Gold Standard” marker. High homocysteine is a major red flag that the methylation cycle is “broken,” even if standard B-vitamin tests look fine.
Pediatric B12, Folate, and Homocysteine Reference Range
Marker Lab “Normal” Range Optimal Target for ADHD and Focus Vitamin B12 200 – 900 pg/mL B12: 600 – 900 pg/mL Folate (B9) 4 – 20 ng/mL Folate: 10 – 15 ng/mL Homocysteine 5 – 15 µmol/L Homocysteine: Below 7 or 8 µmol/L
6. RBC Magnesium
Magnesium acts as the body’s natural relaxant, calming the nervous system and regulating neurotransmitter release. Children with ADHD often deplete magnesium more quickly due to higher stress responses and metabolic rates.
When magnesium levels are low, the brain struggles to pause or relax, creating the familiar “wired but tired” sensation.
What to Ask Your Pediatrician
Request an RBC Magnesium (Red Blood Cell Magnesium) test. Standard “Serum Magnesium” tests only measure the 1% of magnesium in the blood; the RBC test measures the magnesium inside the cells, where it actually does its work.
Pediatric RBC Magnesium Reference Range
Age Group Lab “Normal” Range (mg/dL) Optimal Target for ADHD and Focus 1–6 years 4.2 – 6.8 RBC Magnesium: 6.0 – 6.5 mg/dL 7–12 years 4.2 – 6.8 RBC Magnesium: 6.0 – 6.5 mg/dL 13–18 years 4.2 – 6.8 RBC Magnesium: 6.2 – 6.5 mg/dL
7. Diabetes Profile (Fasting Glucose, HbA1c, Insulin)
Blood sugar instability can mimic or worsen ADHD symptoms. Glucose spikes and crashes often produce impulsivity and poor focus.
Children with unstable blood sugar may experience stronger stimulant “crashes” or inconsistent medication effects.
What to Ask Your Pediatrician
Request a Diabetes Profile to evaluate glucose stability and metabolic health:
- Fasting Glucose: Measures baseline sugar levels after an overnight fast.
- HbA1c (Hemoglobin A1c): Reflects average blood sugar control over the past 2–3 months.
- Fasting Insulin: Helps identify Insulin Resistance early, which can cause sugar crashes even if the glucose numbers look “normal.
Pediatric Blood Sugar Reference Range
Marker Lab “Normal” Range Optimal Target for ADHD and Focus Fasting Glucose 70 – 99 mg/dL 80 – 90 mg/dL HbA1c (3-Mo Average) 4.0% – 5.6% 4.8% – 5.2% Fasting Insulin 2.6 – 24.9 uIU/mL 2.0 – 6.0 uIU/mL
🔗 Related Reading:
If your child is constantly fidgeting or unable to relax at night, mineral balance may play a role. Therefore, you may want to explore this guide: Magnesium for ADHD in Children: Can This Mineral Calm Hyperactivity?
What the Research Says: Connecting Biology to Behavior
When we view ADHD through a biological lens, it’s not only a behavioral condition but also a chemical one. Pediatric research shows that specific nutrients act as the keys to neurotransmitter production; when those keys are missing, the brain struggles to regulate attention and mood no matter how much behavioral management is applied.
Key findings from clinical research
1. Thyroid Conditions-ADHD-like symptoms
A 2024 study published in BMC Neurology reported that individuals with hyperthyroidism often experience symptoms nearly identical to ADHD, including anxiety, irritability, and physical restlessness.1
Furthermore, 2020 research found that children born to mothers with hypothyroidism were significantly more likely to receive an ADHD diagnosis, highlighting the strong genetic and hormonal link between thyroid health and focus.2
2. The Dopamine-Iron Link in ADHD
Multiple studies, including a 2018 study published in Nature3 and a 2020 meta-analysis of 17 studies,4 have confirmed that children with ADHD often show lower serum ferritin levels, suggested that iron deficiency may affect attention and behavior.
3. Zinc and ADHD: Connection to Medication Efficacy
Study published in nature, reported that people with ADHD often have lower zinc levels compared to those without ADHD.5
Clinical trials have shown that children with zinc deficiencies often require higher doses of stimulant medication to see a benefit. Because of this, a zinc test is essential before ADHD medication is prescribed.
By correcting a zinc gap first, many parents find that their child’s medication works more smoothly and is effective at a lower, more comfortable dose.6
4. Vitamin D Deficiency and ADHD Symptoms
In 2024, research published in Biological Psychology reported that children with ADHD have significantly lower Vitamin D levels compared to their neurotypical peers. This deficiency leaves the brain “underpowered” for emotional regulation, highlighting Vitamin D’s critical role in mood stability and focus.7
5. MTHFR Gene and ADHD Connection
In a 2022 review, researchers found that genetic variants in the MTHFR gene can reduce the body’s ability to use folate and vitamin B12 effectively. This disruption leads to elevated homocysteine levels, which interfere with neurotransmitter production and emotional regulation.8, 9
6. Magnesium Deficiency and ADHD Link
In 2019, a meta‑analysis published in Psychiatry Research found evidence of an inverse relationship between serum magnesium levels and ADHD. In other words, children with ADHD were more likely to show magnesium deficiency, reinforcing the importance of screening magnesium as part of ADHD evaluation and management.10
7. Blood Sugar & ADHD Link
A 2022 systematic review found a bidirectional link between metabolic health and ADHD: children with ADHD have a higher risk of metabolic issues like Type 1 Diabetes, while those with poor glycemic control (high HbA1c) exhibit more severe inattention and impulsivity.11
How to Talk to Your Doctor (The Script)
“I would like to ensure we have a biological baseline before starting ADHD medication. I want to rule out any nutritional deficiencies or hormonal imbalances that might be mimicking or complicating symptoms. Specifically, could we order a full thyroid panel, serum ferritin, plasma zinc, Vitamin D, RBC magnesium, a methylation panel (B12/Folate/Homocysteine), and a metabolic panel (Fasting Insulin/HbA1c)?“
The Takeaway
ADHD is a complex condition, and medication is often only one part of care. While it can be life-changing, it does not address underlying medical issues—such as thyroid imbalance or nutrient deficiencies—that may affect attention, mood, or sleep.
Reviewing key blood tests for ADHD in children provides a clearer picture of overall health. This approach may help:
- Improve Accuracy: Identify medical “mimics” like iron deficiency (ferritin) or thyroid dysfunction that can resemble ADHD.
- Support Treatment: Ensure nutrient levels such as zinc and magnesium are sufficient to support brain function and focus.
- Promote Safer Care: Addressing blood sugar or nutrient gaps may help children tolerate medication more comfortably and reduce side effects.
Ultimately, this approach goes beyond symptom management to support a child’s overall neurological health and development.
Frequently Asked Questions (FAQ) About ADHD Blood Tests
Q1. Can ADHD be detected by a blood test?
No. ADHD is diagnosed through clinical evaluation and behavioral history. However, doctors may order blood tests to rule out medical conditions such as thyroid imbalance, iron deficiency, or vitamin deficiencies that can mimic ADHD symptoms.
Q2. Why do I need a blood test for ADHD before starting medication?
ADHD blood work helps rule out conditions like thyroid imbalance, iron deficiency, or vitamin D deficiency that can look like ADHD. Addressing these first can improve how the brain responds to medication and reduce side effects.
Q3. What is the ADHD test called?
There is no single “ADHD blood test.” ADHD is assessed through psychological and clinical evaluations. Blood tests such as thyroid, ferritin, zinc, vitamin D, B12/folate, homocysteine, magnesium, and blood sugar are used as supportive tools to check for underlying medical issues that may influence symptoms or treatment response.
Q4. What vitamin deficiency is linked to ADHD?
Deficiencies in Vitamin D, B12, and minerals like Iron, Zinc, and Magnesium are most commonly linked to increased ADHD symptoms. These nutrients act as “co-factors,” meaning the brain cannot physically manufacture or regulate focus-chemicals like dopamine and serotonin without them.
Q5. Which blood markers are most important for ADHD?
Seven essential markers to review include: Thyroid Panel, CBC + Ferritin (iron stores), Zinc, Vitamin D, Vitamin B12 & Folate (with Homocysteine), RBC Magnesium, and a Diabetes Profile. These directly affect neurotransmitter production, regulation, and overall brain function.
Q6. What are the side effects of ADHD medication and nutrient deficiency?
When nutrient deficiencies are not corrected, ADHD medication may cause stronger side effects such as irritability, sleep disturbances, appetite changes, or “medication crashes.” Ensuring adequate iron, zinc, vitamin D, B12, folate, and magnesium levels helps the brain tolerate medication more smoothly.
Q7. Can low iron or vitamin D cause ADHD symptoms?
Deficiencies don’t cause ADHD, but low iron or vitamin D can intensify inattention, hyperactivity, or mood swings. Correcting these imbalances often improves focus, emotional regulation, and overall treatment success.
Q8. What is a normal ferritin level for child with ADHD?
While standard laboratory reference ranges may list anything above 15 ng/mL as ‘normal,’ research suggests that for children with ADHD., ferritin levels below 50 ng/mL may be associated with increased symptom severity. Many functional practitioners aim for a target range of 50 to 90 ng/mL to ensure the brain has adequate iron stores for dopamine synthesis.
Q9. Do these tests replace behavioral evaluation for ADHD?
Pediatric blood work for ADHD is a complementary tool. It ensures the brain has the right nutritional and hormonal foundation for treatment but does not replace the clinical and behavioral evaluation performed by a psychiatrist or pediatrician.
Q10. What happens if deficiencies are found?
Your doctor may recommend supplementation, dietary changes, or referrals to specialists (e.g., endocrinology for thyroid issues). Correcting deficiencies often makes ADHD medication more effective and better tolerated.
Q11. Can children and adults both benefit from ADHD blood tests?
Yes. Both children and adults with ADHD benefit from checking these markers, especially if symptoms are severe, medication responses are unpredictable, or family history suggests thyroid or nutrient issues.
References
📚 Click to view references
- Chen G, Gao W, Xu Y, Chen H, Cai H. Serum TSH Levels are Associated with Hyperactivity Behaviors in Children with Attention Deficit/Hyperactivity Disorder. Neuropsychiatr Dis Treat. 2023 Mar 7;19:557-564. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC10007977/
- Peltier MR, Fassett MJ, Chiu VY, Getahun D, et al. Maternal Hypothyroidism Increases the Risk of Attention-Deficit Hyperactivity Disorder in the Offspring. American Journal of Perinatology. 2021;38(02):191–201. Available from: https://www.thieme-connect.de/products/ejournals/abstract/10.1055/s-0040-1717073
- Tseng P-T, Cheng Y-S, Yen C-F, Chen Y-W, Stubbs B, Whiteley P, et al. Peripheral iron levels in children with attention-deficit hyperactivity disorder: a systematic review and meta-analysis. Scientific Reports. 2018;8:788. Available from: https://www.nature.com/articles/s41598-017-19096-x
- Anand B, Sireesha CV. Lower serum ferritin levels and higher inattentiveness in attention deficit hyperactivity disorder in a case–control study. Archives of Mental Health. 2022;23(2):95–100. Available from: https://journals.lww.com/amhe/fulltext/2022/23020/lower_serum_ferritin_levels_and_higher.4.aspx
- Ghoreishy SM, Ebrahimi Mousavi S, Asoudeh F, Mohammadi H. Zinc status in attention-deficit/hyperactivity disorder: a systematic review and meta-analysis of observational studies. Scientific Reports. 2021;11:14612. Available from: https://www.nature.com/articles/s41598-021-94124-5
- Rosenau PT, van den Hoofdakker BJ, Matthijssen AFM, van de Loo-Neus GHH, Buitelaar JK, Hoekstra PJ, Dietrich A. Withdrawing methylphenidate in relation to serum levels of ferritin and zinc in children and adolescents with attention-deficit/hyperactivity disorder. Journal of Psychiatric Research. 2022;152:31–37. Available from: https://www.sciencedirect.com/science/article/pii/S0022395622003119
- Miller MC, Pan X, Eugene Arnold L, Mulligan A, Connor S, Bergman R, deBeus R, Roley-Roberts ME. Vitamin D levels in children with attention deficit hyperactivity disorder: Association with seasonal and geographical variation, supplementation, inattention severity, and theta:beta ratio. Biol Psychol. 2021 May;162:108099. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC8187333/
- Meng X, Zheng JL, Sun ML, Lai HY, Wang BJ, Yao J, Wang H. Association between MTHFR (677C>T and 1298A>C) polymorphisms and psychiatric disorder: A meta-analysis. PLoS One. 2022 Jul 14;17(7):e0271170. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC9282595/
- Yektaş Ç, Alpay M, Tufan AE. Comparison of serum B12, folate and homocysteine concentrations in children with autism spectrum disorder or attention deficit hyperactivity disorder and healthy controls. Neuropsychiatr Dis Treat. 2019 Aug 6;15:2213-2219. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC6689552/
- Effatpanah M, Rezaei M, Effatpanah H, Effatpanah Z, Varkaneh HK, Mousavi SM, Fatahi S, Rinaldi G, Hashemi R. Magnesium status and attention deficit hyperactivity disorder (ADHD): A meta-analysis. Psychiatry Res. 2019 Apr;274:228-234. Available from: https://pubmed.ncbi.nlm.nih.gov/30807974/
- Ai Y, Zhao J, Liu H, Li J, Zhu T. The relationship between diabetes mellitus and attention-deficit hyperactivity disorder: A systematic review and meta-analysis. Frontiers in Pediatrics. 2022;10:936813. Available from: https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2022.936813/full
