Is your child hyperactive at bedtime just when it’s time to wind down?
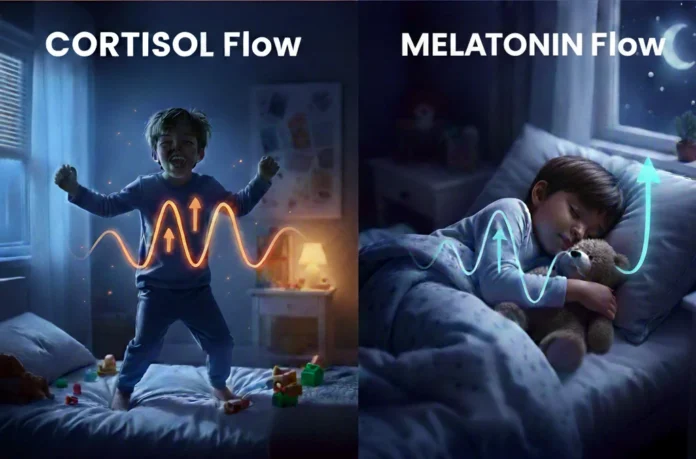
This bedtime hyperactivity is common in kids ages 3 -10, and it’s not just “bad behavior. It often happens due to a timing mismatch between two key hormones: Cortisol and Melatonin. Recent research and data from the National Heart, Lung, and Blood Institute (NHLBI) show that the balance between these hormones is critical for helping kids transition into deep, restorative sleep.
If this imbalance continues over time, it can affect more than just bedtime struggles—it may disrupt overall sleep quality, mood regulation, and even daytime focus and learning. That’s why understanding the cortisol–melatonin connection is so important.
In this guide, you will learn the science behind how cortisol and melatonin interact, along with practical, science-backed strategies to restore hormonal balance, helping calm a hyperactive child at bedtime and support healthy sleep.
Bedtime Hyperactivity in Children: The Cortisol–Melatonin Connection
Under normal conditions, a child’s sleep is regulated by two primary hormones
- Cortisol (The “Alert” Hormone): Peaks in the morning to help us wake up.1
- Melatonin (The “Sleep” Hormone): Rises in the evening to prepare the body for rest.2
When these two hormones work in harmony, bedtime becomes predictable and calm. But when a child misses their natural sleep window (a 30–60 minute period when the brain is primed for rest), the brain registers the extreme fatigue as a state of stress.3
In response, it triggers a nocturnal cortisol spike while simultaneously blocking melatonin.
The Result: This cortisol surge acts like a powerful, unwelcome stimulant, keeping the brain on high alert. Instead of winding down, elevated cortisol directly blocks melatonin. This leads to:
- Bedtime Resistance (the “wired but tired” effect).
- Shallow and Fragmented Sleep
- Frequent child night wakings.
This biological mismatch explains why your child is hyperactive at bedtime instead of sleepy. Their body is chemically “locked” in alert mode, making it physically impossible for them to settle down until the cortisol surge fades.
Signs Your Child Is Overtired at Bedtime
Bedtime hyperactivity may look like misbehavior, but it’s often a sign your child’s body is overtired. Watch for these cues:
- Sudden Energy Spikes: Your child gets a “burst” of energy or starts running around just when they should be sleeping.
- Hyper-verbal behavior: Getting silly, loud, or talking nonstop.
- Resistance: Fighting pajamas, brushing teeth, or getting into bed.
- Emotional Fragility: Becoming more emotional or easily upset over small things.
- Loss of coordination: Tripping, stumbling, or dropping things more often.
- The “Wired” Look: Trouble settling even when their eyes look exhausted.
Common Triggers That Keep Kids Wired at Night
In most cases, even when parents set up bedtime routines, certain everyday habits can keep cortisol levels high, leaving kids wired instead of sleepy. Here are the most common triggers:
- Screen time before bed: Tablets, TVs, and phones emit blue light that mimics daylight. This delays melatonin release and keeps cortisol elevated.
- Stress or overstimulation: Busy evenings, loud environments, or emotional stress can some time triggers a “fight or flight” stress response, spiking cortisol.
- The Sugar-Cortisol Loop: Sometime late sugary or processed foods give kids a burst of energy and spike cortisol levels. Read our 2026 Research Update: Does Sugar Actually Cause Hyperactivity? to see how glucose impacts the brain.
- Irregular routines: Skipping consistent bedtime rituals confuses the body’s natural rhythm, making it harder for melatonin to rise.
- Late-Night Vigorous Play: While physical activity is vital, but vigorous play close to bedtime can keep cortisol high.
How to Lower Cortisol and Support Melatonin (Ages 3–10) for Better Bedtime Sleep
To stop a child from being hyperactive at bedtime, we have to physically signal the body to switch from “Alert Mode” to “Rest Mode.”
Here are four science-backed strategies to flush out cortisol and help melatonin rise:
Strategy The Action The Biological Why Protein Bridge High-protein snack at 3:00 PM (Eggs, nuts, or yogurt). Prevents a blood sugar crash and the cortisol spike that blocks sleep. Heavy Work 5 minutes of “Animal Crawls” or “Wall Pushes” Lower Cortisol: Deep pressure (proprioception) grounds the nervous system Biological Sunset Dim lights or use amber tones 60 minutes before bed Boost Melatonin: Prevents blue light from blocking sleep hormone production Temperature Drop Warm bath followed by a slightly cooler bedroom Trigger Sleepiness: Mimics the natural body temperature drop needed for rest
1. The Protein Bridge: The 3 PM Connection

Steady blood sugar helps prevent bedtime energy spikes.
Many children reach for sugary snacks around 3 PM after school, but those quick bursts of energy can disrupt the body’s natural rhythm.
- The Science: A high-sugar snack after school can cause a blood sugar crash by 5:00 PM, triggering a cortisol surge that later prevents melatonin (the sleep hormone) from rising at bedtime.
- Solution: Offer a protein‑rich snack (like boiled eggs, peanut butter with apple slices, pumpkin seeds or Greek yogurt). These options keep blood sugar steady and help prevent the late‑day cortisol spike.4 For more focus-boosting ideas, see the Best Diet for ADHD Kids: 5 Iron-Rich Superfoods.
2. Use “Heavy Work” Activities (Proprioceptive Input)

When kids are “wired,” their bodies are actually searching for ways to calm down. Deep pressure and resistance activities—known as heavy work—help the nervous system shift into rest mode.
- The Science: These activities provide proprioceptive input: pressure and resistance that signal the brain to release calming chemicals and reduce stress hormones.5
- Try Deep Pressure Activities: Just 5 minutes of simple activities can make a big difference:
- Animal Crawls — crawl with hands and feet
- Wall Pushes — press palms firmly against the wall for resistance
- Laundry Train — push a laundry basket filled with clothes
- Pillow Sandwich — gently press a pillow over the child’s body (avoiding the face) while they lie on the floor.
For more playful ideas, see our full guide on Toddler Activities and Routines, where you will find additional ways to help children regulate their energy and calm their nervous system.
3. The 60-Minute “Biological Sunset”

Dimming lights 60 minutes before bedtime helps mimics the natural sunset and prepares your child’s body for sleep.
The pineal gland in the brain is highly light-sensitive. Bright overhead LEDs, tablets, or TVs give off blue light that mimics midday sun, keeping cortisol levels high and delaying sleepiness.
- The Science: Evening exposure to blue light interferes with the conversion of serotonin into melatonin,6 delaying melatonin release.
- Try this: Switch to warm‑toned lighting — such as amber or red bulbs — at least 60 minutes before bedtime. This “dimming” effect mimics sunset and signals the brain to release melatonin, helping your child transition naturally into sleep.
4. The Temperature “Drop” Method

A drop in core body temperature is a primary biological trigger for sleepiness.
- The Science: As your child’s body temperature falls, it signals the brain to slow down the metabolic rate and prepare for rest.
- Try this: Give your child a warm bath 60–90 minutes before bed. When they step out into a slightly cooler room, the rapid evaporation of water from the skin causes their core temperature to drop, triggering a natural melatonin release.
Bedtime Hyperactivity and ADHD: Red Flags Parents Should Know
If your child is consistently wired at bedtime despite calming routines, it may be a sign of sensory processing differences or an underlying neurodivergent trait such as ADHD. While occasional bedtime restlessness is common, consistent struggles can point to deeper patterns worth exploring.
Red Flags of Early ADHD Signs in Kids (Ages 3–10):
- Persistent bedtime struggles: Hyperactivity every night, even with consistent routines.
- Daytime challenges: Ongoing issues with focus, impulsivity, or emotional regulation.
- Sensory sensitivities: Strong reactions to noise, textures, or transitions that make winding down harder.
- Neurodivergent traits: ADHD or sensory processing differences can amplify bedtime hyperactivity.
What Parents Can Do Next
Step 1. Make 7‑Day Pre‑Evaluation Log
If these ADHD red flags sound familiar, shift from worrying to observing. Use our 7-Day Pre-Evaluation Log to record bedtime behaviors, wake‑ups, and daytime focus.
 Download Your FREE 7-Day Behavior Observation Log PDF
Download Your FREE 7-Day Behavior Observation Log PDF
Click the link below to get your professional, printable PDF version of the ADHD Early Signs Tracker.
[Download the 7-Day ADHD Behavior Observation Log (PDF) Here]
This log is not a diagnostic tool for ADHD. Instead, it provides your pediatrician or specialist with a clear “data map” of behavior patterns.
Step 2. Rule Out the Mimics
Sometimes ADHD‑like behaviors are caused by other conditions. Before assuming ADHD, talk with your doctor about possible medical mimics:
- Thyroid imbalance: In some children, an overactive thyroid (hyperthyroidism) can speed up the body’s metabolism, causing internal restlessness, a racing heart, and “wired” energy that looks identical to hyperactivity. See full related article here: Is It ADHD or a Thyroid Condition? 7 Hidden Signs of Misdiagnosis in Children.
- Iron deficiency: Sometime low iron can cause restlessness and poor focus. See full related article here: Is It ADHD or Iron Deficiency? 7 Hidden Signs to Avoid Misdiagnosis.
- Magnesium deficiency: Magnesium is the “calming mineral.” When levels are low, the nervous system stays in a state of high alert, making it difficult for a child to physically relax or transition into sleep at night. See full related article here: Magnesium for ADHD in Children: Can This Mineral Calm Hyperactivity? (2026 Update).
Step 3: Consult a Specialist for a “Sensory Sleep Plan”
If your log shows ongoing patterns and medical mimics are ruled out, it’s time to seek professional guidance.
A pediatrician, sleep specialist, or occupational therapist can design a personalized sensory sleep plan that addresses your child’s unique neurological needs.
The Takeaway: Your 3-Step Bedtime Reset
When a child is hyperactive at bedtime, it’s usually a sign of overtiredness, not misbehavior. Missing the natural sleep window raises cortisol — the body’s stress hormone. High cortisol blocks melatonin, the sleep hormone, leaving children wired instead of sleepy.
You can not discipline a hormonal spike, but you can manage it. By working with your child’s biology, you signal the nervous system that it’s safe to power down. Try these three steps:
- DIET: Offer a protein‑rich snack around 3 PM to keep blood sugar steady and prevent late‑day cortisol spikes.
- MOVE: Use 5 minutes of “heavy work” (like bear crawls or wall pushes) to physically lower cortisol and calm the nervous system.
- DIM: Switch to warm lighting about 60 minutes before bed to support melatonin release and mimic the natural sunset.
- COOL: Use the temperature‑drop method — a warm bath followed by a cooler room — to trigger natural sleepiness.
The Bottom Line
Small, consistent changes can calm a child hyperactive at bedtime and build a healthier sleep rhythm. They give your child the deep, restorative sleep needed for healthy growth, learning, and emotional balance.
👉 Start with just one step tonight to begin shifting bedtime from chaos to calm.
Frequently Asked Questions (FAQ)
Q1. Why is my child hyperactive at bedtime?
Bedtime hyperactivity is usually a sign of overtiredness. When children miss their natural sleep window, the body triggers a rise in cortisol (the stress hormone). This blocks melatonin (the sleep hormone), leaving them “wired” instead of sleepy.
Q2. Is bedtime hyperactivity a sign of ADHD?
Not necessarily. While many children experience “second winds” due to biology, consistent bedtime hyperactivity is a common trait of ADHD. If these spikes are paired with daytime impulsivity or focus challenges, it may be worth discussing a sensory-based sleep plan with a pediatrician.
Q3. How can I calm a child hyperactive at bedtime?
Use the Move, Dim, Cool framework: 5 minutes of “heavy work” (like bear crawls or wall pushes) to lower cortisol, dimming lights 60 minutes before bed to protect melatonin, and a warm bath to trigger a core temperature drop.
Q4. What is the best bedtime routine for kids who get “wired” at night?
The best routine focuses on sensory regulation. Beyond just “quiet play,” incorporate proprioceptive input (deep pressure) and a “biological sunset” (amber-toned lighting). Consistency is key to training the brain’s circadian rhythm.
Q5. Does screen time make bedtime hyperactivity worse?
Yes. Blue light from screens suppresses the pineal gland’s ability to release melatonin. This creates a chemical “alert” signal in the brain, making it nearly impossible for a hyperactive child to settle for at least 60–90 minutes after use.
Q6. How do I know if my child is overtired or just misbehaving?
Overtiredness has physical markers: dilated pupils, increased talking speed, and clumsiness. These are biological symptoms of rising cortisol. If the behavior only appears during transitions or late evening, it is likely a hormonal “second wind,” not intentional misbehavior.
Q7. What age group is most affected by bedtime hyperactivity?
Children ages 3–10 are the most affected. During these years, children are often dropping naps or starting school, which makes their “sleep window” much narrower and their nervous systems more sensitive to cortisol spikes.
Q8. When should I seek professional help for bedtime hyperactivity?
If sleep struggles affect your child’s daytime learning or if these routines don’t provide relief, consult a specialist. Keeping a 7-Day ADHD & Sleep Symptom Tracker can help your pediatrician determine if the issue is a simple hormonal mismatch or a sensory processing difference.
References
📚 Click to Expand Citation
- Brum MCB, et al. (2022). Andreadi A, Andreadi S, Todaro F, Ippoliti L, Bellia A, Magrini A, Chrousos GP, Lauro D. Modified Cortisol Circadian Rhythm: The Hidden Toll of Night-Shift Work. Int J Mol Sci. 2025 Feb 27;26(5):2090. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC11899833/
- Wong SD, et al. (2022). Development of the circadian system in early life: maternal and environmental factors. J Physiol Anthropol. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC9109407/
- Juliana N, et al. (2025). Cortisol Detection Methods and the Hormone’s Role in Evaluating Circadian Rhythm Disruption. Int J Mol Sci. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC12470794/
- Pattnaik H, et al. (2022). Nutritional Elements in Sleep. Cureus. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC9859770/
- Guardado KE, Sergent SR. (2023). Sensory Integration. StatPearls [Internet]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559155/
 Download Your FREE 7-Day Behavior Observation Log PDF
Download Your FREE 7-Day Behavior Observation Log PDF