Recognizing early signs of ADHD in toddlers is not always simple. Young children are naturally curious, energetic, and impulsive. But when a child’s activity feels “driven by a motor” or begins to disrupt family routines and safety, many parents wonder: Is it normal development, or could it be a sign of something deeper?
Before you worry, understand this: many high-energy behaviors are completely normal milestones at this age. This guide helps you notice patterns, not label your child.
ADHD is a neurodevelopmental condition that affects focus, self-regulation, and behavior. The key difference is not just the amount of energy—it is how the developing brain manages and directs that energy.
Quick ADHD Prevalence Stats:
- 11.4% of children (3–17): Have received an ADHD diagnosis (CDC survey).
- 1.4% of toddlers (3–5): Are diagnosed early; however, a formal diagnosis at this age is uncommon.
- The Gender Gap: Boys (~15%) are nearly twice as likely to be diagnosed as girls (~8%)
- Co-occurring Conditions: Nearly 78% of children with ADHD have at least one other condition, such as anxiety (39%) or behavior problems (44%).
Toddler Development vs. ADHD Symptoms: The Biological Reality
To tell the difference between a high-energy child and ADHD symptoms, we need to look at how behavior shows up in daily life. A toddler’s brain is still developing. Therefore, many behaviors that resemble ADHD are actually normal for ages 2 to 3.
Normal Toddler Milestones (The Baseline)
In a typically developing toddler, high energy is usually a tool for learning. It usually looks like this:
- Purposeful Activity: Their energy has a clear goal. They run because they want a specific toy; they climb because they want a snack.
- Impulsivity: They may rush toward danger, but usually stop when told “No” or “Stop.”
- Growing Attention Span: A 3-year-old can focus for about 6–8 minutes on a preferred task; a 4-year-old often manages 8–12 minutes.
- Big Emotions: Small frustrations (like a broken cracker) trigger big reactions because the emotional brain develops faster than the logical brain.
- Predictable Transitions: While they may protest, most 4-year-olds can switch from play to meals with consistent routines.
The “ADHD Difference”
Clinicians become concerned when behaviors are:
- persistent,
- unusually intense, and
- present across multiple settings such as home, daycare, and play environments.
Most toddlers show some of these behaviors at times. However, patterns that continue over months matter more than isolated incidents.
The Key Distinction: Typical toddler energy is purposeful and goal-oriented, whereas ADHD-related hyperactivity often appears aimless, is commonly described as being “driven by a motor,” and continues across all settings even when the child is exhausted.
While a typically active child can “hit the brakes” when prompted, a child with ADHD traits struggles because their brain’s impulse control system is not fully engaging.
To make this easier to see, here’s a side-by-side look at typical toddler patterns compared with ADHD-linked concerns.
Feature Typical Toddler ADHD Red Flag Movement Purposeful & goal-led Aimless & "motor-driven" Impulses Responds to "Stop" No brakes"; repeats risks Focus Brief but engaged Derailed by any noise Emotions Resets quickly Intense; slow to "reset" Bedtime Natural "off switch" More "wired" when tired Sleep Restful & consistent Delayed melatonin; frequent wakes Setting Varies by location Same behavior everywhere
ADHD Symptoms by Age (2 to 5 Years)
To identify early signs of ADHD in toddlers, it helps to look at how behavior changes as the brain develops. Use the following guide to spot these patterns.
Age Typical Development ADHD-Related Concerns 2 Years Climbs to reach a specific toy. Constant, aimless climbing/running. 3 Years Can stay with one toy for 5+ mins. Shifts toys every 30–60 seconds. 4 Years Stops running when called. No brakes"; repeats risks after warnings. 5 Years Sits for short "circle time." Cannot sit still or follow 2-step directions.
Signs of ADHD in 2 year olds: The “Motor Always On” Stage
At age two, high energy is usually purposeful and curiosity-driven. ADHD symptoms in 2-year-olds may include:
- Aimless Movement: Running or climbing without a clear goal.
- Persistent Risk-Taking: Repeating dangerous behaviors even after correction.
- Intense Meltdowns: Tantrums that are longer and more frequent than peers.
Signs of ADHD in 3 year olds: The “Impulsivity Peak”
Most three-year-olds can follow simple rules. ADHD-related signs at this age include:
- Rapid Task-Switching: Moving from toy to toy every 30–60 seconds.
- Sensory Distractibility: Easily pulled away by minor background noise.
- Low Frustration Tolerance: Extreme meltdowns triggered by small changes.
Signs of ADHD in 4 year olds: The “Gap Between Energy and Control”
By age four, children usually start “hitting the brakes.” Signs of ADHD appear when energy outpaces control:
- Developmental Lag: Energy of a preschooler but impulse control of a younger toddler.
- Cross-Setting Behavior: Hyperactivity is equally intense at home, daycare, or the park.
- Difficulty with Transitions: Struggling to move from one activity to another, even with warnings.
Signs of ADHD in 5 year olds: The “School Readiness Stress Test”
The demands of starting school can make ADHD symptoms more noticeable.
- Classroom Challenges: Difficulty sitting for circle time or following multi-step instructions.
- Social Interference: High-intensity play that disrupts peers or leads to frequent interventions.
- The “Second Wind”: Persistent hyperactivity at night, becoming more restless as they tire.
The Science: What Makes an ADHD Brain Different?
Understanding why these behaviors happen helps replace stigma with biological clarity.
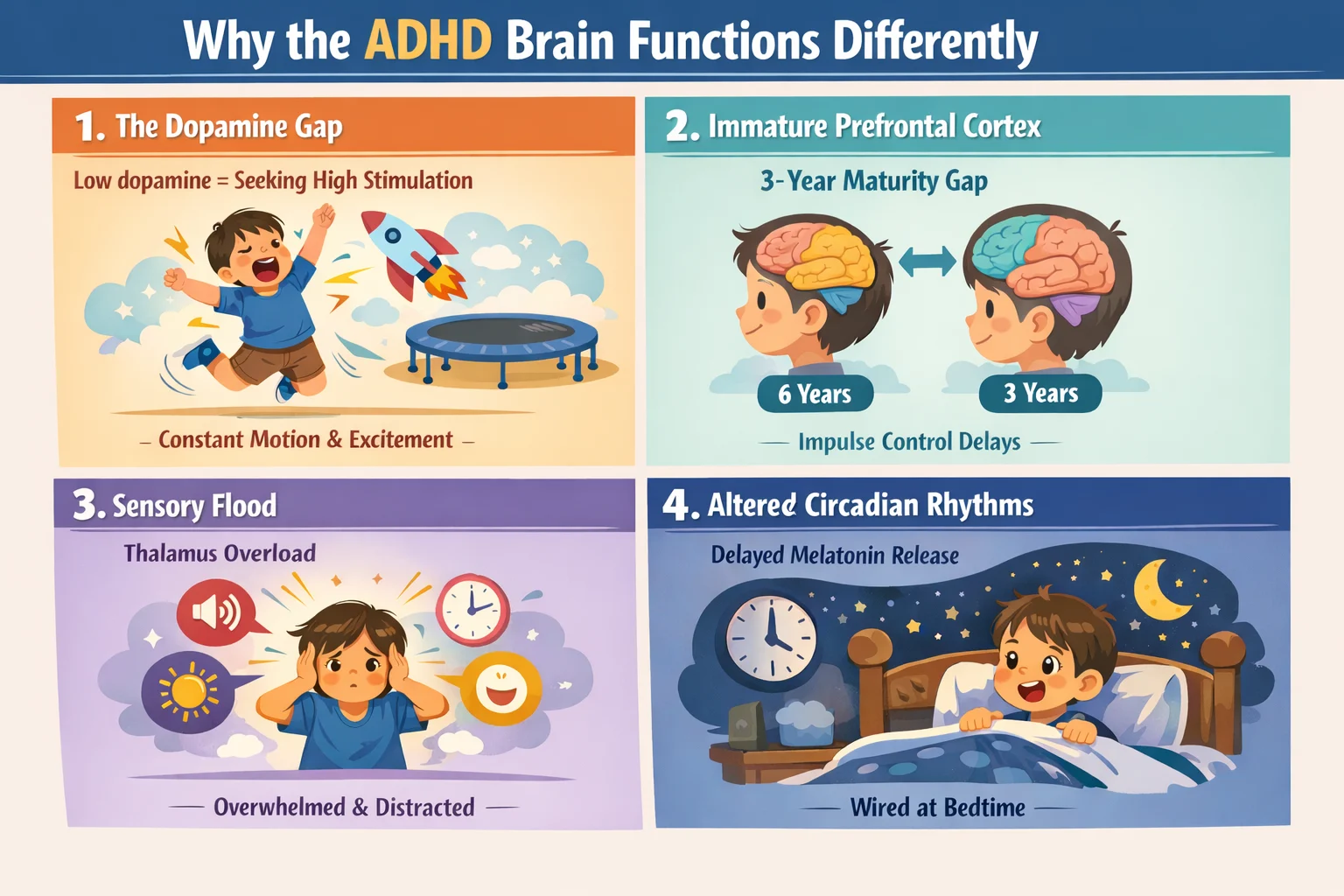
1. The Dopamine Gap: Why ADHD Toddlers Seek High Stimulation
Dopamine is the neurotransmitter responsible for motivation, focus, and reward.1 In children with ADHD-like patterns, dopamine signaling is less efficient.
- The Result: The brain feels “under-stimulated.”
- The Behavior: To activate their focus centers, children instinctively seek “high-octane” activities like jumping, shouting, or constant movement.
2. The Maturity Gap: Limbic System vs. Immature Prefrontal Cortex
The Limbic System (emotions) matures early, while the Prefrontal Cortex (the “CEO” or brakes) matures later.2 In children with ADHD, the prefrontal cortex can mature more slowly than expected, with a developmental delay of up to about three years.
- The result: A “developmental gap” where a child’s age and energy level progress faster than their brain’s ability to regulate impulses and behavior.
- The Behavior: A 4-year-old may have the physical energy of a preschooler but the impulse control of a 2-year-old.
3. Sensory Flood: Why Background Noise Feels Overwhelming
A typical brain has a “filter” (the Thalamus) that ignores background noise, like the hum of a refrigerator. In the ADHD brain, the “gate” stays wide open.3
- The Result: Sights, sounds, and sensations all compete for the child’s attention at the exact same intensity.
- The Behavior: This “sensory flood” leads to the rapid switching of tasks and the extreme distractibility parents observe during play. The child is not “ignoring” you; they are simply unable to pick your voice out of the environmental noise.
4. Circadian Delay: The Bedtime “Second Wind”
Melatonin is a sleep hormone that helps regulate the body’s sleep–wake cycle.4 Many hyperactive toddlers experience a delay in melatonin release.
- The Result: Their biological clock runs late, so an 8:00 PM bedtime feels like 4:00 PM.
- The Behavior: Instead of winding down, toddlers become wired—hyperactive, talkative, and restless at night.
7 Neurological ADHD Red Flags in Toddlers to Watch For
If you notice these seven signs appearing consistently for more than six months, it may indicate a need for behavioral interventions.
1. Movement “Driven by a Motor”
Children with early ADHD traits often moves aimlessly and constantly. This “motor-like” restlessness continues even during quiet activities like meals or story time, with no natural “off switch.”
2. The “No Brakes” Phenomenon
While all toddlers are impulsive, a red flag is a persistent inability to stop even after clear, repetitive guidance. This may look like:
- Running into traffic or unsafe areas suddenly.
- Repeating risky behaviors immediately after an injury.
- Finding it extremely difficult to wait, even briefly
3. Profound Distractibility (The Filtering Gap)
The ADHD brain struggles to filter “background noise.” A toddler may
- Rapid switching between activities
- Strong sensitivity to background noise
- Difficulty staying with even preferred tasks
4. Prolonged Emotional Dysregulation
Tantrums are part of normal development, but ADHD‑linked meltdowns tend to be:
- More intense than typical outbursts
- Triggered by small frustrations
- Harder to recover from, even with comfort
5. Trouble Slowing Down at Night
Instead of winding down, some children with ADHD traits become more “wired” as they get tired. The brain seeks stimulation to fight off sleepiness, leading to:
- More excited: Rather than calming, they grow more hyper and impulsive.
- Physical restlessness: Even in bed, they may talk incessantly, fidget with blankets, or get up repeatedly.
- Hypersensitivity: Small sounds or minor changes in the room wake them easily because their brain stays on high alert.
6. Biological Sleep Disruptions
Molecularly, ADHD is often linked to delayed melatonin onset. These children may
- Wake frequently,
- Struggle to fall asleep for hours, or
- Appear hyperactive during the day due to poor restorative sleep
7. The “Universal” Pattern
ADHD patterns are universal. If ADHD like behaviors (running, jumping, etc.) appears consistently across multiple environments such as:
- At home,
- At daycare or preschool, or
- At the park or with friends
Parent Note: If a child is only hyperactive at home but perfectly calm at daycare, the issue may be environmental or sensory rather than neurological.
Wait—Is it ADHD or a “Mimic”?: Other Conditions That Look Similar
Before confirming early signs of ADHD in toddlers, clinicians must rule out “Medical Mimics.”—conditions that produce identical behaviors. Addressing these first ensures your child gets the right kind of support.
- Thyroid Dysfunction: An overactive thyroid (hyperthyroidism) can cause internal restlessness, irritability, and a racing heart.5 (Related: Is It ADHD or a Thyroid Condition? 7 Hidden Signs of Misdiagnosis in Children)
- Mineral Deficiencies: Iron, Magnesium, and Zinc are essential for dopamine production. If these levels are low, the brain can not “focus”, cam and regulate emotions.6 (Related: Is It ADHD or Iron Deficiency in Children? 7 Hidden Signs to Avoid Misdiagnosis)
- Sensory Processing Issues: Some children are “sensory seekers.” They may crash into things, jump constantly, or spin. This is not just hyperactivity. Instead, their nervous system is trying to get enough body awareness input to feel balanced.7
- Sleep Apnea: Enlarged tonsils or snoring can disrupt sleep. As a result, daytime adrenaline surges may cause hyperactivity that mimics ADHD.8
- Hearing or Language Delays: A child who can not process what is being said may appear inattentive or “spaced out.”
When to Talk to a Pediatrician
Doctors are often cautious about diagnosing ADHD before age 4. Still, you should seek an evaluation promptly if you notice these four critical signs:
1. Safety is a Constant Issue
- What it means: While all toddlers take risks, a red flag is when impulsivity overrides survival instincts.
- The Sign: Your child regularly puts themselves in danger such as bolting into traffic, jumping from dangerous heights, or touching hot surfaces despite repeated, clear corrections.
2. Daily Life is Heavily Disrupted
- What it means: When the neurological noise becomes so loud that normal life stops, it is time for a professional opinion.
- The Sign: Everyday activities like grocery shopping, eating out, or visiting friends feel nearly impossible. If you find yourself avoiding normal outings to prevent meltdowns, it’s time for professional input.
3. Persistent Social Struggles
- What it means: Toddlers are still learning to share, but ADHD like patterns can make peer interaction extremely difficult.
- The Sign: Your child consistently has trouble playing with others, is frequently too rough, or is unable to follow even the simplest group flow, leading to isolation from playgroups or daycare.
4. Chronic Sleep Deprivation
- What it means: Many children with ADHD experience a delay in melatonin release, which disrupts their natural sleep cycle.
- The Sign: Ongoing difficulty falling or staying asleep is affecting your child’s daytime mood and your family’s ability to function. If everyone is living in a state of exhaustion, a medical rule out like a sleep study or mineral check is necessary.
Parent Note: Bringing your 7-Day Observation Log helps your doctor see the patterns that a short office visit might miss.
The Takeaway
Recognizing ADHD traits in a 3-year-old is not about labeling a “bad kid”—it’s about understanding a brain that is wired differently. With strategies like heavy work, visual schedules, and co-regulation, you are not just managing behavior; you are supporting your child’s brain toward balance.
If you have concerns, noticing these patterns early is the first step toward a calmer, more manageable daily routine. Remember: seeking clarity early is not a weakness—it’s one of the most powerful tools a parent can give their child.
Frequently Asked Questions (FAQ)
Q1. At what age does ADHD start to show?
Signs of ADHD in toddlers often become noticeable between ages 3 and 5. This is when children are expected to follow simple rules, sit for short group activities, and manage transitions better. ADHD traits stand out when a child’s energy, impulsivity, and distractibility remain much more intense than peers and do not improve as the brain matures.
Q2. Can ADHD be diagnosed before age 4?
ADHD is rarely diagnosed before age 4, and formal diagnosis under age 3 is especially uncommon. A toddler’s brain develops rapidly and unevenly, so many behaviors that look like ADHD symptoms can still fall within normal development. Most pediatricians therefore focus on tracking behavior patterns over time and using supportive strategies, such as behavioral therapy, rather than labeling toddlers with ADHD too early.
Q3. What are the most common early signs of ADHD in toddlers?
The most common early signs include constant, aimless movement (feeling “driven by a motor”), an inability to stop even when in physical danger, extreme distractibility in quiet settings, and meltdowns that are significantly more intense than typical tantrums.
Q4. How do you know if your child has ADHD?
There is no single medical test for ADHD. Instead, professionals evaluate behavior patterns across multiple settings like home and daycare. They also rule out “medical mimics,” such as hearing issues or nutrient deficiencies. Keeping a 7-Day Behavior Log is the best way to provide your doctor with the objective evidence needed for an accurate evaluation.
Q5. How do I know if my toddler’s hyperactivity is normal or ADHD?
Typical toddler energy is usually goal-oriented (running to reach a toy). In contrast, ADHD-related hyperactivity often feels aimless and chaotic, persists even when the child is exhausted, and occurs consistently across all environments, including the park and daycare.
References
📚 Click to view citations
- Gold MS, Blum K, et al. Low dopamine function in ADHD: should genotyping signify early diagnosis? Postgrad Med. 2014. View on PubMed
- El-Baba RM, Schury MP. Neuroanatomy, Frontal Cortex. StatPearls [Internet]. 2023. View NCBI Bookshelf
- Batty MJ, et al. Morphological abnormalities in prefrontal surface area and thalamic volume in ADHD. Psychiatry Res. 2015. View PMC Article
- Luu B, Fabiano N. ADHD as a circadian rhythm disorder: evidence and implications for chronotherapy. Front Psychiatry. 2025. View PMC Full Text
- Chen G, Gao W, Xu Y, Chen H, Cai H. Serum TSH Levels are Associated with Hyperactivity Behaviors in Children with Attention Deficit/Hyperactivity Disorder. Neuropsychiatr Dis Treat. 2023 Mar 7;19:557-564. View on PubMed
- Robberecht H, Verlaet AAJ, Breynaert A, De Bruyne T, Hermans N. Magnesium, Iron, Zinc, Copper and Selenium Status in Attention-Deficit/Hyperactivity Disorder (ADHD). Molecules. 2020 Sep 27;25(19):4440. View on PubMed
- Maćkowiak I, Ciesielska J, Ruszczyk M, Opydo-Szymaczek J, Torlińska-Walkowiak N. Sensory Processing Disorder in Children-Description of the Phenomenon and Practical Procedures. J Clin Med. 2025 Jun 10;14(12):4105. View on PubMed
- Nguyen-Thi-Phuong M, Nguyen-Thi-Thanh M, Goldberg RJ, Nguyen HL, Dao-Thi-Minh A, Duong-Quy S. Obstructive Sleep Apnea and Sleep Disorders in Children with Attention Deficit Hyperactivity Disorder. Pulm Ther. 2025 Sep;11(3):423-441. View on PubMed